What is the pelvic floor?
Pelvic floor muscle and anatomy illustrations used with permission from Pelvic Guru and Your Pace Yoga
When we refer to the pelvic floor, it is often a shortcut to refer to the muscles that make up the pelvic basin. The pelvic floor also includes:
blood vessels
nerves
ligaments
fascia
fatty tissue
lymph
skin
This is all within the border of the pelvis.
Bony landmarks of the pelvis
The pelvic girdle is comprised of two halves to the pelvis, called innominate, which are made up of three fused bones:
pubis
ilium
ischium
Connecting these two pelvic halves in the back of the body are the sacrum (triangular bone at base of spine) and coccyx (tailbone).
There is a cartilage joint at the front of the pelvis that completes the pelvic ring called the pubic symphysis. This can get quite painful for some women during their pregnancy.
Where is the pelvic floor?
Pelvic floor from the back
Let’s map out the area where your pelvic floor lives. If you are comfortable touching the bones that create the border as described above, please do. If not, just imagine where they are.
Find your pubic bone in the front of your pelvis.
Reach around to the very bottom of your spine where your tailbone (or coccyx) is (hint: it’s usually lower than we may think).
If you are sitting, lift your right butt cheek and find your sitz bone (or ischial tuberosity).
You have now mapped out the diamond shape of the bottom of your pelvis. Within this bony border you will find all of your pelvic floor muscles!
The pelvic floor muscles are comprised of three layers.
Layer 1 of the pelvic floor
First layer of pelvic floor muscles with vulvovaginal anatomy
This layer is the outermost layer. This layer has four muscles that can be palpated both externally and internally.
These muscles can be palpated internally on women and people with vulvovaginal anatomy at the dept ofhen one finger-knuckle-length. For those with penile anatomy these muscles will be palpated externally:
Bulbocavernosus/bulbospongiosus
Ischiocavernosus
Superficial transverse perineal
External anal sphincter
This layer helps to close around all of the tubes at the end of the urinary system (urethra), gastrointestinal system (anus), and the reproductive system (vagina for those who have them).
Additionally, this layer allows for sexual function with the erectile tissues of the clitoral and penis.
The tissue between the vagina and anus is called the perineal body. This tissue might suffer a tear during childbirth. Physical therapy while pregnant and after childbirth can help with this!
Layer 2 of the pelvic floor
Second layer of pelvic floor muscles with vulvovaginal anatomy
The closure around the tubes continues with layer 2. This layer is referred to as the deep perineal pouch.
It’s less obvious to pinpoint where the muscles are as compared the first and third layers, but for women with urinary urgency you can trigger this sensation when you palpate the compressor urethra muscle.
This layer is palpated at the depth of the second knuckle on the index finger . The muscles are:
Urethral sphincter
Deep transverse perineal
Compressor urethra (vulvovaginal anatomy only)
Sphincter urethrovaginalis (vulvovaginal anatomy only)
Layer 3 of the pelvic floor
Third layer of the pelvic floor muscles with vulvovaginal anatomy
This layer is the innermost layer of the pelvic floor muscles. This layer is also referred to as the pelvic diaphragm.
This muscular sling looks like a hammock, acting to provide support for the bladder, rectum, and for those who have one, a uterus.
This layer has a right and left side:
Pubococcygeus
Iliococcygeus
Coccygeus
This layer is co-contracts with the deepest layer of the abdominal wall to act as core support and provides support for our pelvic organs.
Pelvic wall muscles
Not to be ignored are two important muscles that make up the pelvic walls: the piriformis and obturator internus.
The piriformis muscle is a hip external rotator (think turned out like a ballet dancer). It often gets press for causing pain in the sciatic nerve when it’s overactive or tight, but the problem could be with the obturator internus, which is also a hip external rotator. (The pelvic specialists reading this now have a magical glow about them. We love this muscle.)
The obturator internus is very often a culprit in deep vaginal, rectal or hip pain. Pelvic specialists love this muscle because when we palpate it, the patient will often say, “Yes, that’s exactly my pain. No one has been able to find that before.”
Hip rotators
Illustration courtesy of Pelvic Guru. Used with permission.
So, if you experience what you think is sciatica, it might actually be your obturator internus irritating your sciatic nerve, not the piriformis. The sciatic nerve is the cream in the Oreo cookie between the piriformis and the obturator internus and can be irritated by either muscle.
Lengthen and strengthen: action steps for pelvic pain and incontinence
What do we focus on with our pelvic floor when we experience pain or incontinence?
If you experience any type of pelvic pain, you will want to release muscle holding, tightness, and spasm in the pelvic floor. This is called “downtraining” because we are looking to encourage the sympathetic nervous system (fight or flight) to downregulate and ask the pelvic floor muscles to relax and lengthen.
If your goal is to decrease urinary or fecal leakage, reduce or prevent pelvic organ prolapse, decrease back or hip pain, or optimize core control, you will want to strengthen the pelvic floor. This is called “uptraining,” which means we are encouraging the pelvic floor muscles to strengthen so they can engage along with the rest of the core musculature.
Downtraining pelvic floor muscles
When we look at releasing tension and lengthening the pelvic floor muscles we have a lot of tools in our toolbox.
Awareness
Now that you understand where the pelvic floor is and what it does, you can start to build more awareness.
Notice during the day if you find yourself holding during stressful moments. Notice if you find yourself holding while you are trying to elongate during a bowel movement.
Most of my patients find it helpful to reference this breath cues sheet to practice releasing tension during the day and incorporate it into movement, stretching, or a yoga home program.
Pelvic health physical or occupational therapy
It’s important to visit a primary care provider, urologist, gynecologist or urogynecologist first to make sure there isn’t a non-musculoskeletal cause of your symptoms. After you are cleared, you can see a pelvic health physical therapist (PT) or occupational therapist (OT).
Your pelvic rehab therapist will assess for:
strength, weakness or over-activity of musculature
flexibility and tissue pliability
movement impairments and retrain for optimal neuromuscular coordination and control
myofascial and visceral restrictions
Core stability exercise
Dilator training
I wrote a blog on how you can use mindfulness while working with dilators.
This helps reprogram the brain from assuming the pelvic floor is a dangerous zone. Even if you are “relaxed,” the unconscious brain might try and protect you if there was previous pain in this region by creating tension in the muscles.
There is a free guided meditation at the end of this blog too!
Yoga and breathwork
Illustration courtesy of Pelvic Guru. Used with permission.
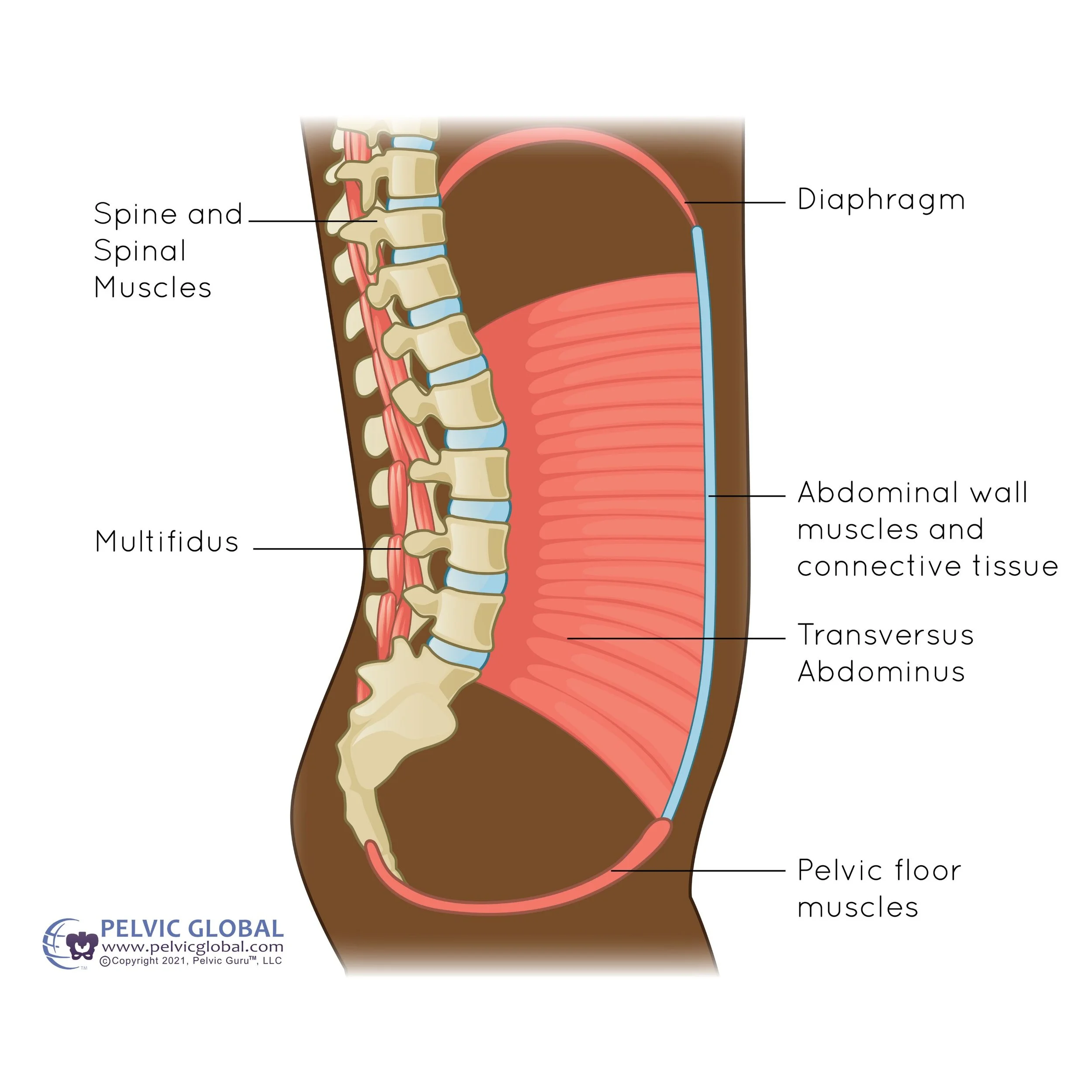
Relationship between diaphragm and pelvic floor
I’m linking these strategies together because they all have one thing in common: you!
You don’t need your PT or OT. You don’t need a piece of equipment. You have everything within you!
Your diaphragm has a direct relationship with your pelvic floor muscles. We can use breath and mindfulness to influence the nervous system and pelvic floor.
You’ll find lots of postures on my website you can explore, and also read more about pranayama, or breathwork.
Uptraining the pelvic floor muscles
Once you are feeling better and have less pain, you might start to work carefully to strengthen. Talk to your therapist about how to best approach that plan!
For those of you who aren’t recovering from pain and are looking to strengthen your pelvic floor muscles, you may want to explore Kegels.
There are three phases of rehab I think of when I’m helping guide someone to get stronger in the pelvic floor:
Awareness
Learning where and how the pelvic floor muscles are is the first step in strengthening.
Building awareness through education, like looking at pelvic models (shout-out to #penelopethepelvis) and anatomy photos, will help you find the muscles.
Other ways to build awareness is through observation of contractions while looking in a hand mirror, palpation of the muscles while practicing contractions, and biofeedback (external or internal sensor).
Isolation
In regards to training the pelvic floor muscle, I think of it in three steps:
create awareness of where they are
contract them without contracting other muscles (isolate)
integrate into function
Now that you have created awareness about where the muscles are, you can learn to contract them without contracting the other muscles around them. This is isolating the muscle, as opposed to allowing the gluts or inner thighs to help out. Interested in learning how to contract your pelvic floor muscles with different cuing? Be sure to read this blog.
Functional training
In this phase of training we add pelvic floor muscle cues and contractions to movements. The Chair Pose is one example: